New editiorial! Dense granules are released from platelets upon activation. When decrease in numbers or lacking, patients are prone to bleeding. This editorial, together with Prof. Walter Kar describes the pros and cons about current methods and the new JTH paper in this space.

May 2025
New editiorial! Dense granules are released from platelets upon activation. These granules contain many important platelet activating factors (see figure).
When low in numbers or lacking all together in disease, patients are prone to bleeding. In dispite of new technologies and diagnostic tests, these diseases are still not easy to diagnose and specialised laboratories are needed.
This editorial, together with Prof. Walter Kar describes the pros and cons about current methods and the new JTH paper in this space.
NEW paper: Consensus protocol for platelet desialylation

March 24, 2025
It's done! 2 years of work but now finally online here.
Together with my co-PI Alex Kauskot (INSERM, France) we asked the international community about their methods to measure platelet desialylation. The responses were highly variable and protocols not standardised.
Why is this relevant? Platelet contain many carbohydrates (glycans) which can be removed when they're activated in health or in various diseases, see overview here. Especially sialic acid, which is usually capping other glycans, keeping them from binding to various immune cells.
Measuring removal of sialic acid by easy-to-use and cheap flow cytometry method can provide important clues on platelet aging, activation or whether they are rapidly cleared from circulation.
This International Society on Thrombosis and Haemostasis (ISTH) SSC Platelet Physiology paper contains key details to measure this accurately.
It's all about the glycans!
Review on platelet desialylation in health and disease

Platelets are covered with many sugary structures, called glycans. Sialic acid is one of them which covers may other glycans. It can be removed by different enzymes and this process leads to platelet removal from the circulation and activation of platelets.
The invited review on the role of sialic acid (sugar or glycan) removing enzyme, neuraminidase, in platelets, is finally published in Current Opinion in Hematology! I wrote this together with my clinical colleague Dr. Nora Butta. Very proud of the end result with great cartoons also. Apart from clearance, loss of surface sialic acid from the platelet surface affects signaling including ligand binding and platelets procoagulant function. Platelets are also desialylated in bacterial or viral infections, during senescence, various mutations, platelet auto antibodies, hemostasis and shear stress. See here.
Platelet release different extracellular vesicles during their storage
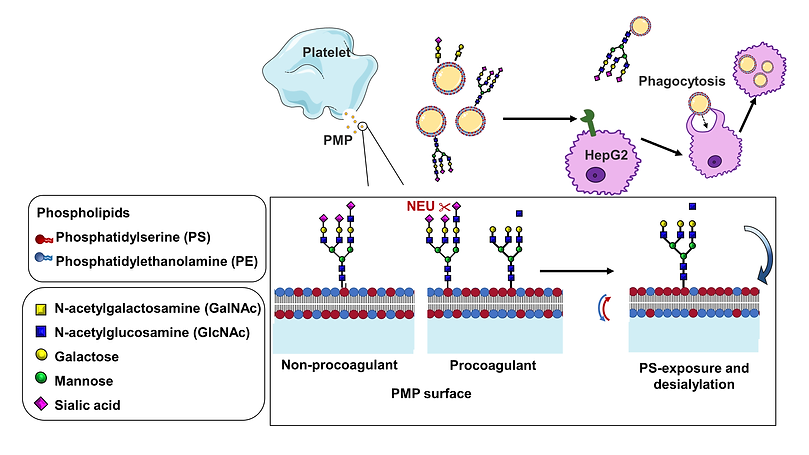
CHANGES IN GLYCANS ON PLATELET MICROPARTICLES RELEASED DURING STORAGE OF APHERESIS PLATELETS ARE ASSOCIATED WITH PHOSPHATIDYLSERINE EXTERNALIZATION AND PHAGOCYTOSIS
April 27, 2022
Platelets release small vesicles (microparticles) during storage. These are important for clotting but also have sugars on their surface which are removed during platelet storage, which are linked to their procoagulant function and clearance from the circulation when transfused. Read here.

DONOR CITRATE REACTIONS INFLUENCE THE PHENOTYPE OF APHERESIS PLATELETS FOLLOWING STORAGE.
Oct, 2021
Accepted in Transfusion! During platelet donation, a small proportion of donors experience adverse reactions, such as citrate reactions: numbness and tingling in the mouth and fingers, with muscle contraction in more severe cases. Apheresis platelets donated by donors that experienced a citrate reaction during donation had a higher platelet activation response and possibly a more procoagulant platelet microparticle phenotype. See Link.
X-IRRADIATION AND GAMMA-IRRADIATION INACTIVATE LYMPHOCYTES IN BLOOD COMPONENTS
Sept, 2021
Blood components are irradiated to prevent transfusion associated graft versus host disease (TA-GvHD) which can result from donor lymphocytes which may persist in the transfused units. Gamma and X-irradiation are known to reduce lymphocyte viability and function. We show that white cell viability and lymphocyte function were similarly affected by X- and gamma-irradiation. This indicated that X-irradiation is a suitable replacement for gamma-irradiation. Read here


PREVIOUS PUBLICATIONS
2020
Receptors on the platelet surface contain many sugars. One of them is sialic acid, which can be removed by enzymes known as neuraminidases. Removal of these sugars can lead to platelet clearance from the circulation.
We show for the first time that when platelets are activated, neuraminidase activity increases, demonstrating a previously unrecognised role for neuraminidases in platelet signalling.
We also show for the first time that NEU1 is present in alpha granules while NEU2 is present in mitochondria.
2020
Nonsteroidal anti-inflammatory drugs (NSAIDs) reduce pain and decrease fever. Apart from aspirin, over the counter NSAIDs including ibuprofen & other medications e.g. paracetamol can also affect platelet function and therefore the quality of donated platelets. In this review, we discuss the rationale of deferring platelet donors from donating when they recently took aspirin or other NSAIDs.
2015
Immune thrombocytopenia (ITP) is a life-threatening bleeding disorder caused by anti-platelet antibodies destroying platelets, leading to low platelet numbers. In ITP different antibodies circulate, against different platelet proteins.
In my first postdoc, together with Prof. Heyu Ni in Toronto, we found that anti-GPIbα (adhesion receptor), but not anti-GPIIbIIIa (aggregation receptor) antibodies, induces Fc-independent platelet activation, sialidase neuraminidase-1 translocation and desialylation.
This leads to platelet clearance in the liver via hepatocyte Ashwell–Morell receptors. This is different from what was previously believed and many ITP treatments target the spleen. 30% of patients don't respond.
Importantly, sialidase inhibitors, similar to Tamiflu, prevented anti-GPIbα-mediated platelet destruction and rescued platelet numbers in a mice model of ITP. Therefore, desialylation could be a potential diagnostic biomarker and therapeutic target in the treatment of refractory ITP.

PhD PUBLICATIONS
The platelet storage lesion (PSL) is one of the key factors that limit the platelet shelf-life to 5 days. Storage of platelets at low temperature reduces bacterial growth and might better preserve the haemostatic function of platelets than current procedures. During my PhD project I studied the effect of cold storage on platelet function.


Cold storage exposes glycan (sugar) residues on platelet's adhesion receptor glycoprotein (GP)
Ibα, inducing rapid platelet destruction by the liver.
When we mimiced cold-storage
and post-transfusion conditions) triggers a conformational change in GPIb. Cold shifts GPIbα from membrane to cytoskeleton, crucial for platelet-platelet clumping (agglutination) and spreading on VWF surface under blood flow.
During cold-storage of platelets and rewarming, scaffolding 14-3-3 proteins associate with GPIbα and dissociate from pro-apoptotic Bcl-2 protein Bad. This initiates apoptosis, leading to platelet phagocytosis by
macrophages. Responses are prevented by clustering inhibitor and removal of GPIbα.
Conclusions: Cold-rewarming triggers apoptosis. Attempts to improve platelet transfusion by cold-storage
should focus on prevention of the GPIbα-change.


Storage of platelets at low temperature reduces bacterial growth and might better preserve their function. However, cold-storage
triggers GPIbα association with scaffolding 14-3-3ζ protein and apoptosis involving release of arachidonic acid (AA).
AA-depletion made platelets resistant against cold-induced cell death and improved platelet survival in a mouse model.
Attempts to improve platelet transfusion by cold-storage should focus on transient AA-depletion.
We report a 70 year old patient with unexplained thrombocytopenia (low platelet count). The patient had easy bruising and a long bleeding time. Her platelets aggregated spontaneously. Patient had developed an auto-antibody against GPIbα, which initiates haemostasis, platelet death, possibly through clustering of GPIbα.


